A nursing professor has produced more than 30 episodes of a podcast the past several months to raise awareness about geriatric nursing, according to a School of Nursing release.
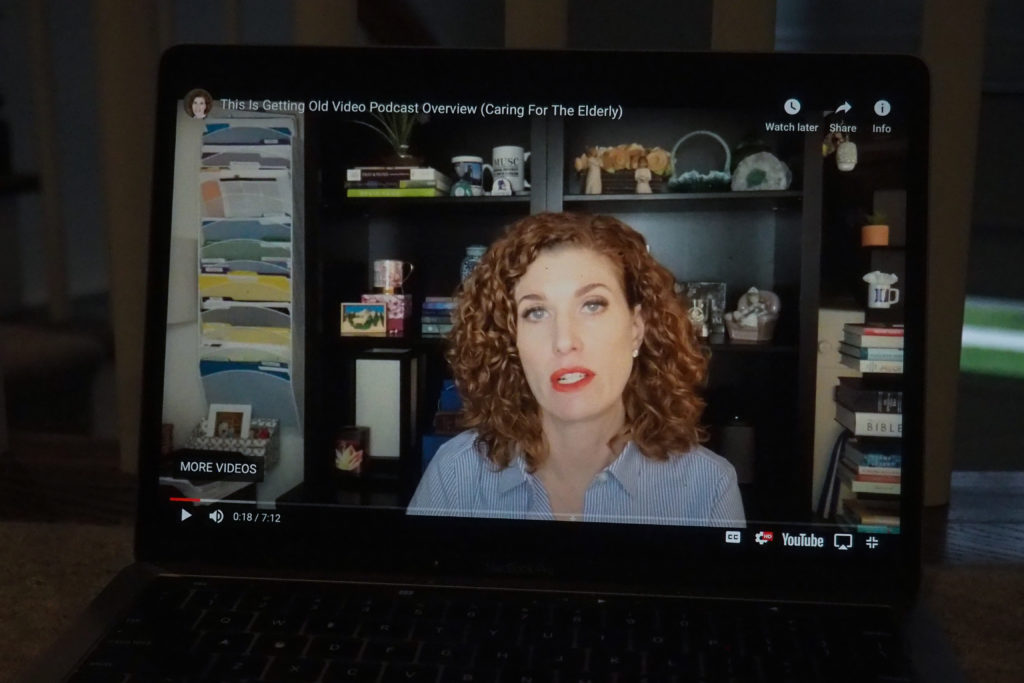
Melissa Batchelor, the director of the Center for Aging, Health and Humanities in the nursing school, said she started the project, titled “This is Getting Old: Moving Toward An Age-Friendly World,” in March to find a way to educate nursing professionals about geriatric nursing. Experts in geriatric nursing said the podcast provides a platform to discuss the complexities of geriatric nursing to communities like nursing students and family caregivers.
Batchelor said she wanted to have an outlet to discuss different topics in nursing, like how nurses can influence health policy and how to discuss COVID-19 with older relatives, and has so far produced more than 30 episodes. She said the podcast, which can be viewed on YouTube, is focused on how to improve geriatric nursing care policies.
“It’s not really about getting old – although sometimes we do talk about aging issues – it’s really more about all of the things, all of this stuff that’s not ready,” Batchelor said. “So that’s what’s getting old. We don’t have better long-term care policies.”
The podcast focuses on a specific topic each week and features interviews with different nursing experts, like nursing professors Ellen Kurtzman and Ashley Darcy-Mahoney. Batchelor said she had worked on a previous podcast about geriatric nursing, which drew about 60,000 listeners from more than 40 countries on YouTube.
“To me, it demonstrates the power of technology because I was like ‘60,000 people are never going to read peer-reviewed publications. They just won’t,’” Batchelor said.
One of the podcast’s more recent episodes, titled “10 warning signs for Alzheimer’s disease,” was picked up by the Alzheimer’s Association from Alaska and has received nearly 300,000 views and more than 3 million interactions across different platforms, making the episode the most viewed segment.
Batchelor said one of her central goals for her podcast is to promote “geriatricized” health care policy — policy that considers the concerns of the elderly. She said she’s planning to put out four episodes on the Age Friendly Health System, a policy initiative that aims to bring care to older adults in the health care system.
“They need to be valued and everybody needs to have a purpose, and there’s a way for us to be intergenerational and interprofessional to make that happen,” she said.
Batchelor said she hopes to promote youth interest in geriatric care through the podcast because the nursing field, especially geriatric nursing, faces a shortage of younger nurses. She said 2 percent – about 65,000 – of the millions of nurses in the United States are board-certified in gerontology.
Batchelor said she’s had conversations with her students interested in mother-baby nursing about how having a knowledge of geriatric nursing can aid grandparents with conditions like Alzheimer’s in safely holding their grandchild.
“How are you going to adjust your nursing care to meet the emotional needs of that family and that older adult to bond with that baby?” Batchelor said.
Experts in geriatric nursing said the podcast is an easy and accessible way to bring awareness to issues within geriatric nursing.
Janet Mentes, a professor of nursing at the University of California, Los Angeles, said the podcast could be most helpful for families or health care providers who want to know how to best care for their older relatives.
“The public should understand about geriatric care because every family has older members, and they should be aware of the special needs of their older relatives, specifically about issues of preventive care and diseases more common in older persons such as dementia,” Mentes said in an email.
Laura Kirk, a clinical associate professor of nursing at the University of Minnesota, said she hopes the podcast will allow the public to understand the role that geriatric nurses have to aid elderly populations.
“What nurses actually do and are capable of doing is lost on/hidden from the general public,” she said in an email. “To the extent that nurses, particularly advanced practice nurses, are well suited to assist in the management of chronic co-morbid illness and disability, public understanding and buy-in is important.”
Terri Harvath, the director of the University of California Davis Family Caregiving Institute, said understanding the unique experience that older adults face with illness can help nurses better care for that population. She said older adults often experience a cough or raised heart rate as symptoms of an illness, whereas younger adults typically show signs of illness with severe fatigue or a high fever.
“Sometimes in nursing we overstep our bounds and prioritize our view of safety above the patient’s autonomous views of what’s in their best interest,” Harvath said. “And I think that if she could focus on issues where there is dynamic tension between safety and autonomy and quality of life to really deepen our understanding of how complex those issues are.”