Researchers at GW’s Public Health Lab are fundraising to develop free, at-home sexually transmitted infection tests for students.
Jack Villani, the laboratory’s manager, said at-home STI collection kits will allow GW students to privately collect swab samples of their throats, genitals and rectums and return them to the lab to test for STIs like chlamydia and gonorrhea. He said the lab — which currently processes COVID tests — will refer students with positive tests to the Student Health Center and hopes the system will reduce the social stigma surrounding sexual health.
Villani said the lab is currently seeking up to $500,000 in funding to cover the cost of supplies and labor to process the tests so officials can offer the tests to students. Villani said the release date of the kits depends on when the lab receives funding and that the team is currently seeking out a “funding opportunity” from the Centers for Disease Control and Prevention, as well as other federal funding sources.
“We believe that this type of testing is of greatest benefit when there is no cost to the individual so, ideally, we would like to have this project be fully funded and not require any payment from the individual,” Villani said in an email.
A CVS-brand STI kit for gonorrhea, chlamydia and trichomoniasis costs $89.99, according to the CVS website.
GW would be the only one of its 12 peer schools to offer free, at-home STI test kits. John Hopkins University School of Medicine offers at-home STI test kits for no charge.
Villani said the lab’s STI collection kits will offer testing for chlamydia and gonorrhea, among others, in the throat and rectum, which will address a “public health concern” because STIs can spread asymptomatically through those areas and the “standard” chlamydia and gonorrhea test only samples urogenital specimens. He said the DC Health and Wellness Center, which provides care and treatment for STIs in the District, only tests for chlamydia and gonorrhea using a urogenital sample, meaning the lab’s STI kits will expand access to sexual health services in D.C.
“These sites are considered neglected for screening for STIs but are believed to be commonly responsible for asymptomatic transmission,” Villani said. “With this in mind, we can design our kits to include these sites and help address this public health gap.”
Villani said college students experience STIs at a higher rate than the general population. He said the kits the lab is developing would help “capture” asymptomatic cases when people are unknowingly spreading an STI, since many asymptomatic cases go undetected.
D.C. has the 17th-highest STI incidence rate of all U.S. cities, with 1,393 cases per 100,000 people, according to a CDC report. One in four college students have an STI, and 80 percent of afflicted individuals are asymptomatic, according to a study by Washington and Lee University.
“It’s a major public health concern in D.C. and in any urban center and a passion project for me and a lot of other people here at GW,” Villani said.
The lab staff said on top of their STI research, the lab processes 300 COVID tests per week, a decline from about 3,000 tests per day last academic year. Villani said the decrease in COVID tests allowed the lab “more bandwidth” to begin developing the STI kits in summer 2022.
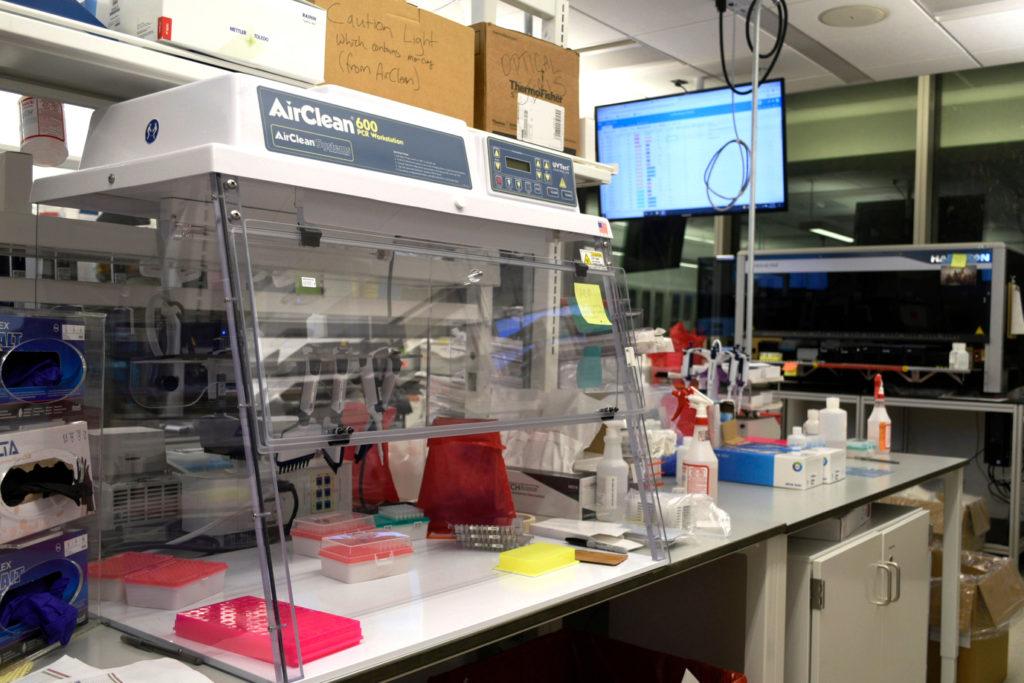
Jorge Sepulveda, the lab’s medical director, said the lab team is trying to “leverage experience” in creating other at-home test kits to adapt their lab infrastructure’s robotic pipetting — robots that measure and move liquids — for other forms of large-scale disease testing, like STI screening. He said lab staff hope more people will opt to get tested for STIs because at-home tests eliminate the need to see a physician unless they receive a positive test.
“That’s sometimes a big barrier to getting tested, and there’s a lot of asymptomatic infection,” Sepulveda said. “If we can remove this barrier, it will hopefully have a positive impact.”
The CDC recommends anyone who engages in risky sexual behavior, sexually active women younger than 25 and men who have sex with men should be tested annually for gonorrhea and chlamydia. Men who have sex with men should also test for all STIs “more frequently” if they have multiple or anonymous partners, according to the CDC.
The CDC does not offer a recommendation for annual STI screening for men who have sex with women, citing “insufficient evidence” for regular testing among men at “low risk” for STIs.
DC Health provides free, confidential, at-home and in-lab STI tests for District residents ages 13 and up through Get Checked D.C., a program providing HIV and STI testing to D.C. residents, according to the agency’s website.
Maddy Niziolek — a co-president of GW Reproductive Autonomy and Gender Equity, a student organization for reproductive justice and sex positivity — said on-campus access to free, at-home tests would benefit students who don’t have time to visit the SHC, can’t afford a doctor’s appointment or feel a “stigma” from seeing a medical professional for STI testing. Niziolek said at-home STI tests would be helpful to students who previously experienced racism, ableism or misogyny in health care and would prefer waiting to consult a professional until they know if their test came back positive.
The SHC offers STI testing, screening, treatment and counseling by appointment as a primary care service, according to the center’s website.
“They would really be able to fully control their own health and practice autonomy over their own sexual health and be able to test on their own time,” Niziolek said.
Yuka Manabe, the director for the Center for Innovative Diagnostics for Infectious Diseases at Johns Hopkins University and current leader of I Want The Kit — a program established in 2004 that provides free at-home STI tests for the state of Maryland as well as nine other states through the Indian Health Service — said offering at-home testing is particularly helpful for women, whose STIs are often asymptomatic. About 50 percent of women with gonorrhea and 70 percent of women with chlamydia experience no symptoms, according to the American Society for Microbiology.
Manabe said the program is helpful in expanding access to STI testing as some of the highest-risk groups are less likely to have health insurance and at-home STI tests from drugstores can be expensive.
“You have to increase the ways that people can get access because not everyone wants to go to an STI clinic and sit there and wait,” Manabe said.