Long COVID-19 is prevalent among 36 percent of GW community members who tested positive for COVID between July 2021 and March 2022, according to a study released last month from the Milken Institute School of Public Health.
Researchers surveyed a sample of 1,338 community members who were infected with COVID during that period and determined 36 percent experienced common long COVID symptoms like fatigue and shortness of breath. Experts in long COVID said the study’s results may influence students’ COVID behavior, like increasing mask-wearing, but the effects and prevalence of long COVID will remain unclear until it receives more national attention and research.
Megan Landry – the study’s lead researcher and the director of the Campus COVID Support Team, a team of faculty and staff who manage the response to COVID cases on campus – said the idea for the study came after the CCST sent out a self-reported symptom check-in between July 2021 and March 2022 to GW community members who tested positive for COVID on campus to evaluate their symptoms. She said the check-in notified officials that the GW community members may be experiencing symptoms of long COVID if they reported symptoms more than four weeks after the initial COVID infection.
Landry said researchers launched a follow-up email study of the campus community in July 2021 to investigate “persistent” symptoms of long COVID. She said the study found vaccination protects against severe infection and limited symptoms consistent with long COVID – nearly half of the 36 percent of patients with long COVID symptoms were not fully vaccinated, according to the study.
“Our results do suggest that vaccination continues to be very important – not only does vaccination protect against severe initial infection – but is also associated with a lower likelihood of reporting symptoms consistent with long COVID,” Landry said in an email.
Landry said the people with the highest risk for long COVID are those with low vaccination levels against COVID and current and former smokers. More than 45 percent of the community members suffering long COVID were former or current smokers and were “significantly” more likely to report experiencing long COVID symptoms, according to the study.
Long COVID is identified when symptoms, like fatigue, brain fog and cough, continue or develop four weeks after the initial COVID infection, according to the CDC.
Landry said more research into long COVID in the GW community is needed to better understand the prevalence and impact of long COVID. She said few studies look into the prevalence of long COVID in younger populations, but the 36 percent prevalence rate in the GW community falls under the wide range of nationwide research results that have found between 10 to 80 percent of COVID survivors experience long COVID symptoms four weeks after initial infection.
“We did not know what to expect before we examined the rates in our community because so few articles have looked at long COVID among younger populations,” Landry said. “Our results do suggest that even young, healthy populations are vulnerable to long COVID.”
GW is the first of its peer schools to conduct a study of long COVID prevalence on campus. A study released in July 2022 by the University of Southern California, which employed an internet-based national survey, found that 23 percent of people who test positive will experience long COVID.
Vivian Jeckell, a freshman majoring in political communication, said she first tested positive for COVID in January 2022 and experienced long COVID for four months after the initial infection, with symptoms like a fever, cough and difficulty breathing. She said when she tested positive for COVID again in October 2022, her doctor said her lungs were already damaged from the previous infection causing the shortness of breath.
Jeckell said she struggles to breathe when doing physical activities like walking upstairs to classes and taking her self-defense LSPA course. She said she wishes GW would advertise more resources to raise awareness about long COVID and its prevention.
“I think it would be beneficial to the University to showcase some of the effects that long COVID can have on people,” Jeckell said. “It might encourage them to wear their masks more and to talk about the fact that it is a thing and it does exist.”
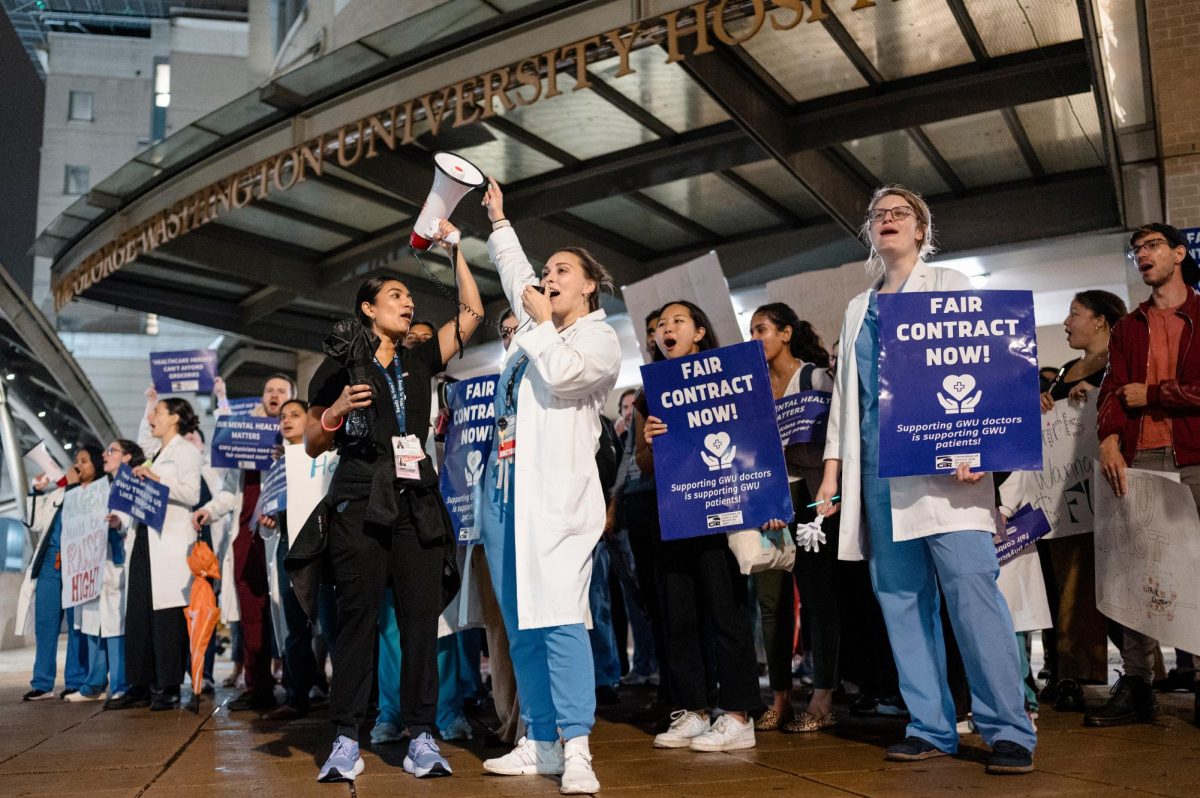
GW’s long COVID recovery clinic opened in the fall of 2020 but closed in June due to staff shortages under the Medical Faculty Associates. The GW Center for Integrative Medicine – GW’s contemporary and alternative medicine practice – is still providing treatment for long COVID through specialized doctors.
Experts in long COVID research said the Milken study adds to a broader understanding of long COVID’s prevalence, but they would like to see more specificity about the definition of long COVID and its symptoms in future studies.
Ziyad Al-Aly, a professor of medicine and clinical epidemiologist at Washington University in St. Louis, said long COVID is an “umbrella term” that includes symptoms like fatigue, brain fog and metabolic disorders like autonomic nervous dysfunction, diabetes and kidney and heart problems that result from COVID infection. He said research trends show that younger adults, like college students, with long COVID are more likely to experience brain fog or fatigue than metabolic disorders.
“I think the core conclusion is that long COVID is not trivial,” Al-Aly said. “It’s significant, it’s important, affecting many, many people and it needs urgent attention.”
Lauren Wisk, a professor in the division of general internal medicine and health services research at the University of California, Los Angeles, said the percentage of individuals with long COVID varies based on preexisting health conditions and vaccination levels, which are common characteristics that are recorded during studies.
She said she hasn’t seen any compelling research into how age affects the severity of long COVID because long-term symptoms among age groups and people with preexisting conditions always vary with most viruses.
“If you’re talking about younger people being impacted with a potentially lifelong, at least long-term chronic condition, the impact for me is greater,” Wisk said. “You have young people who are studying and trying to enter the workforce and begin their careers, and if they have a major impairment, that’s a pretty substantial barrier that they have to overcome at a very critical stage in their life.”