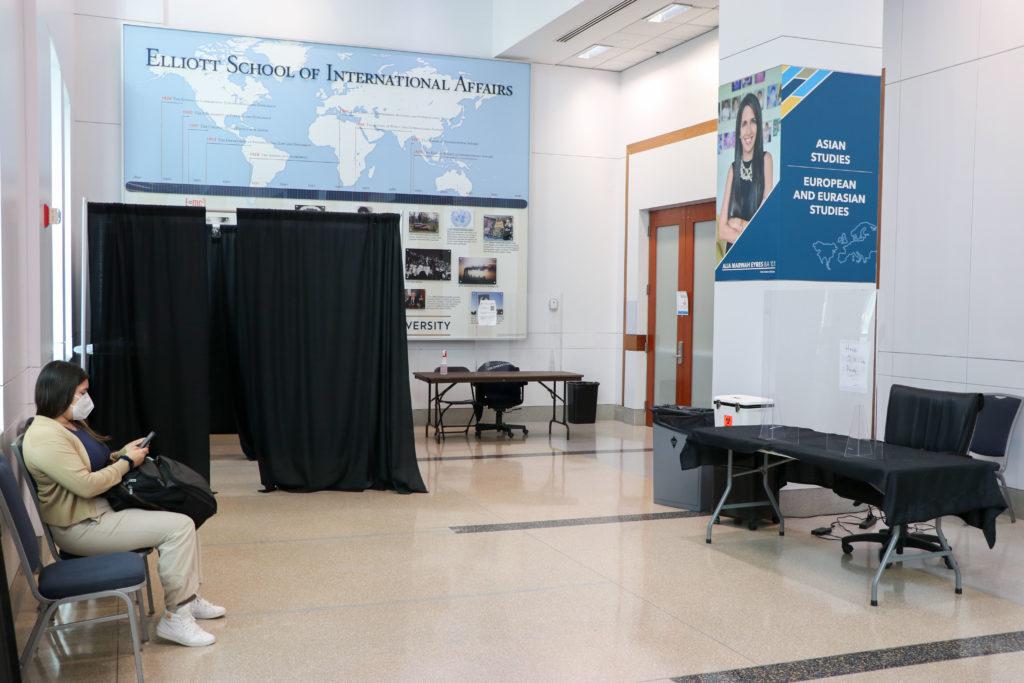
Even after the University eliminated mandatory COVID testing in June, officials are continuing to track case numbers on GW’s dashboard as part of ongoing monitoring efforts that align with all 12 peer schools.
David Diemert, the chair of the GW COVID-19 Medical Advisory Group and a professor of medicine, said the advisory group – the committee composed of faculty experts advising University COVID protocol – is “evaluating” changes to the dashboard because of the increase in individuals using take-home, rapid antigen tests after officials eliminated the biweekly testing requirement. All 12 of GW’s peer schools moved to optional testing, five of which continue to operate their COVID dashboard to track case numbers for the fall semester.
Diemert said the daily positive rate reported on the COVID dashboard does not represent the positivity rate for all GW community members and only represents individuals who chose to test through the University.
At this time last year, more than 33,000 tests were administered with a case positivity rate of 0.6 percent, according to the dashboard. Only about 5,700 tests have been administered so far this fall, with a total positivity rate of about 11 percent.
Diemert said fewer people are using GW’s testing centers after GW made asymptomatic testing optional, and officials will monitor COVID caseloads at GW and in D.C. and the number of COVID patients admitted to hospitals and ICUs to determine COVID protocols. He said there is no absolute threshold of positive cases on campus that would push officials to reinstate the biweekly testing requirement and the advisory group guides the University’s current COVID health protocols on masking, vaccinations and testing by using evidence- and science-based recommendations about COVID protocols.
“Tracking COVID-19 cases helps GW to decide if additional precautions should be instituted if the number of cases starts to climb,” Diemert said in an email.
He said GW takes guidance from the DC Department of Health “very seriously” and works closely with the department to adjust University protocols to changes in case rates. Diemert said the number of positive cases in the D.C. metropolitan area continues to decrease weekly and hospital rates in the D.C. area have consistently declined over the last few months.
DC Health currently classifies the current COVID-19 community level as “low” and has reported no new COVID related hospitalizations in the last two weeks. The Centers for Disease Control and Prevention reports a decrease in average weekly COVID case numbers nationwide, reporting about a 1,000 case decrease per week.
“The MAG has been continuously monitoring the trajectory of COVID-19 globally and locally, and it reviews current data as well as national and local guidance including recommendations from the CDC and the DC Department of Health.” Diemert said.
GW’s 12 peer schools – Boston, New York, Northeastern, Syracuse, Tufts, Tulane, Georgetown and Wake Forest universities, and the universities of Pittsburgh, Miami, Rochester and Southern California – have similar optional testing protocols for the fall semester with all 12 peer schools making testing optional for community members.
Syracuse remains the only university to provide isolation housing for COVID-positive students and also provides vending stations across campus filled with highly subsidized self-administered COVID testing kits for community members.
Experts in medicine said that with the increase in at-home testing for COVID, universities with optional testing requirements need to have clear goals about how they report COVID data.
Robert Ernst – the chief health officer and the associate vice president for student life for health and wellness at the University of Michigan – said the university plans to continue to track COVID data throughout the semester but doesn’t require routine surveillance testing for students and faculty. He said Michigan’s dashboard recently went through an “overhaul” but continues to report transmission rates and identified case numbers.
He said the move to at-home testing represents an “evolution” in the pandemic to a point where individuals, instead of institutions, hold themselves accountable for isolation and testing when exposed. He said people having easy access to vaccines and providing information about how people can protect themselves from COVID are crucial public health strategies for colleges.
“Effective treatments, even for people who get COVID if they’re in a higher risk group, have really changed the ability to protect ourselves,” Ernst said.
He said now that doctors have more of an understanding of COVID, priorities have shifted from rigorous testing and contact tracing when the goal was to know about every single case at the beginning of the pandemic. Ernst said the University of Michigan Medical School implemented a permanent public health response and advisory group instead of an emergency response mode, like what would have been in place in the early stages of the pandemic, to manage the pandemic and other emerging infectious diseases.
“I think the virus has changed over the course of time, but our ability to protect ourselves against COVID has changed also through vaccination, prior infection, more easily accessible high filtration masks,” Ernst said.
Dahlene Fusco, an assistant professor of medicine at Tulane University, said the shift to at-home testing is a pitfall because the CDC doesn’t track results of at-home tests. She said even with university testing, the data needs to be clearly marked with their testing protocols to ensure the data is accurately read.
She said she encourages young people to take control and get tested if they want quicker, more accurate and widespread testing. Fusco said undergraduate students at Tulane started a pop-up PCR testing center out of a residence hall room and encourages any student who has an interest in virology to volunteer at testing centers.
“Don’t wait for mandates, learn how important it is to know what viruses are around so you can nip them in the bud and it’s only when we know what viruses are around that we can develop vaccines and treatments,” Fusco said.