Two researchers from the Milken Institute School of Public Health authored an editorial earlier this month analyzing systemic racism in the health industry, marked by income inequality and a lack of diversity.
The editorial, which the American Public Health Association published in the journal Medical Care, evaluated inequities in pay and access to education which prevent Black, Latino and Indigenous people from accessing jobs and leadership positions in the medical field. The authors propose five evidence-based policies, including plans to recognize the history of racism in medicine, promote policies studying diversity in medical leadership positions and invest in pipeline programs that encourage marginalized communities to enter the medical field.
Anushree Vichare, an assistant professor in the department of health and policy management, and Randl Dent, a research scientist and equity scholar, spearheaded the editorial alongside Jaileessa Casimir, a medical student at the City University of New York.
“It was time to move beyond just describing what the situation is and what the context is and really trying to identify measures that are more actionable,” Vichare said. “It is now time to take action. We’ve done a lot of the talk, now it is really time to do the walk.”
People of color account for 37 percent of healthcare and social assistance workers nationwide, according to the 2020 data from the United States Bureau of Labor Statistics. Only 17.4 percent of workers are Black or African American, and 13.6 percent are Hispanic or Latino according to the bureau.
Vichare said her team’s research is part of a larger effort from people of color in the medical community to address the racist policies and unequal representation still built into the medical system.
“There needs to be a movement in recognizing that the structural racism within the health workforce is not a problem of only physicians and the medical schools,” Vichare said.
She said medical institutions should be held accountable to complete the anti-racist work they pledge to do.
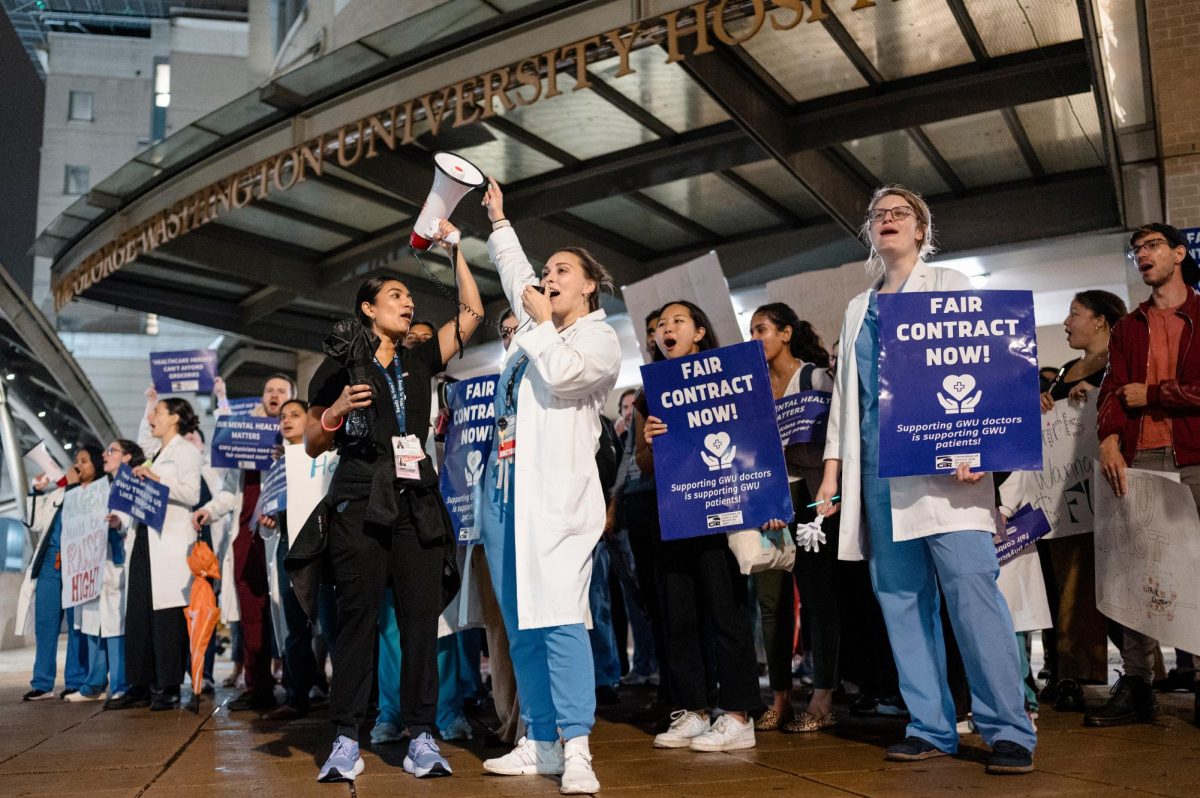
The School of Medicine and Health Sciences formed an anti-racism coalition last summer to address racism and implicit bias, hosting events to educate people on implicit bias and the underrepresentation of minorities in the healthcare workforce.
Dent said the editorial aims to recognize how historically Black colleges and universities have worked to bring physicians of color into the workforce.
The editorial proposes that medical companies invest in schools with Black, Latino and Indigenous students. The authors provide CommonSpiritHealth – a nonprofit medical organization which recently invested in the Morehouse School of Medicine, an HBCU – as an example.
“We really saw that as an opportunity to invest in HBCUs and invest in Hispanic serving institutions that are diversifying the workforce, more than any of the other schools,” she said. “And so that was one of the things that we really wanted to highlight — the schools that are doing it and doing it well.”
She said HBCUs like Howard University College of Medicine, Meharry Medical College and the Morehouse School of Medicine comprise three of the top five schools that graduate the most Black medical students in the country.
Casimir said the authors researched the history of racist medical policies before proposing solutions laid out in the editorial. She said the editorial also discussed the 1910 Flexner Report, a landmark report on medical school higher education that led to the closure of seven of the 10 medical schools that were training Black doctors with limited funding.
“Health structures and inequalities that we experience today is because of what happened in the past,” Casimir said. “How can we dismantle those systems if we don’t even know where their foundation even lies?”
Experts in medicine and public health said structural racism is embedded in the medical system through hiring practices, unequal access to health care facilities and high costs.
Janet Bettger, an associate professor of orthopedics and nursing at Duke University, said the editorial is “extremely important,” because it identifies pipeline programs in high schools targeting students in rural and marginalized communities.
“I appreciated that they were very specific about how they wrote this about pay inequities, about debt, about opportunities, about learning, about discussions,” Bettger said.
Thomas LaVeist, the dean of the Tulane School of Public Health and Tropical Medicine and the former chair of the department of health policy and management in Milken, said the United States is “dramatically” segregated in the medical care industry. He said different racial and ethnic groups receive a varying quality of medical care, and there are fewer health care facilities located near people in rural areas.
“Providers are using the same incentives as other people, and that’s why you see certain communities have an overabundance of health care resources and other communities have essentially no health care resources,” he said.
Sarah Hendrick contributed reporting.