GW’s medical and public health schools collaborate more than any other schools within the University.
A report from the provost at a Faculty Assembly meeting last month showed that the medical and public health schools have the highest number of collaborations on research projects and academic programs. Faculty said cross-collaboration between the two schools can make research projects more competitive for grants and more completely address health problems, like infectious diseases, that involve both policy and medicine.
Officials said the two schools have collaborated on more than 40 sponsored projects with principal investigators since fiscal year 2012.
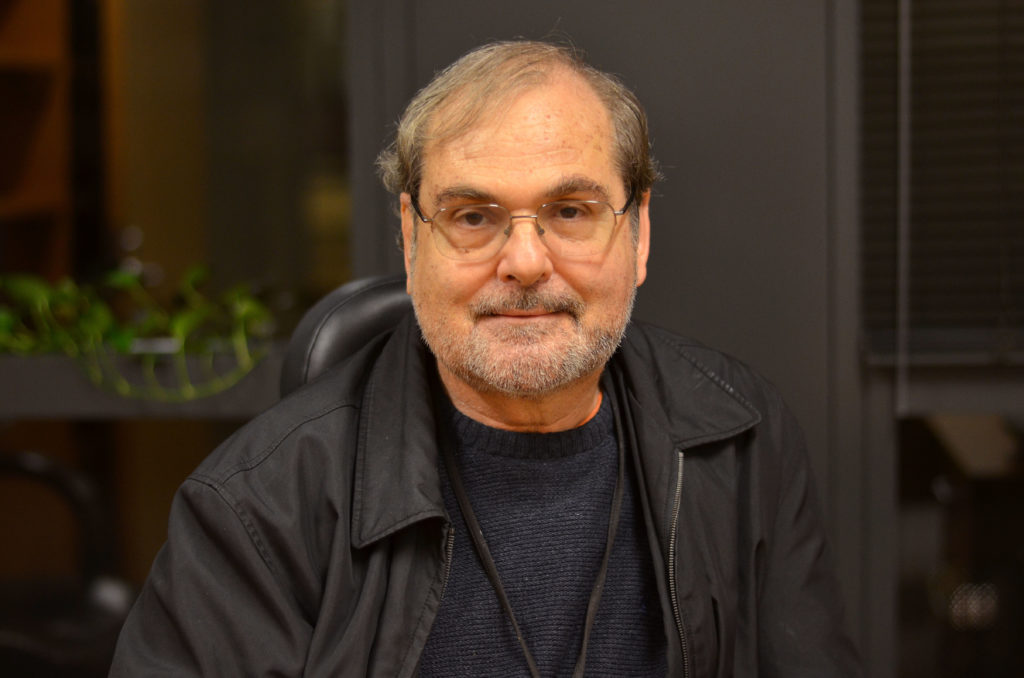
Robert Miller, the vice president for research and the associate dean for research for the School of Medicine and Health Sciences, said the number of collaborations between the two schools is “much higher” than 40 because faculty work together informally in ways that are not captured by metrics and reports on research collaboration.
Miller said officials will continue to “grow and support” interdisciplinary collaboration at GW.
“Collaboration is an integral part of research,” Miller said in an email. “Interdisciplinary research, in particular, cultivates discovery. The result of collaboration is innovative solutions to today’s most complex problems and answers to long-asked questions.”
Fitzhugh Mullan, a professor of health policy and management and of pediatrics, said the Atlantic Fellows for Health Equity program – a program based in GW’s Health Workforce Institute that sends 20 U.S. fellows to other countries each year – works to address issues of health equity.
Mullan said the program brings the work of the medical school and the public health school together to help future doctors develop a deep understanding of health policies and their impact internationally.
“The notion was that a lot of things we do in the school of public health, particularly in the health policy department, were relevant to young doctors and doctors in general because their world is governed in policies,” Mullan said.
Mullan said areas like health care, Medicaid, Medicare, food and drug regulation, and infectious disease control are typically associated with public health but are topics that doctors should also thoroughly understand to ensure quality patient care.
Melissa McCarthy, a professor of health policy and of emergency medicine, said she currently oversees research that looks at the social factors of a patient – like diet and education – which could predict their future health care use and cost under Medicaid. She said her team is currently enrolling patients when they come to the emergency department or visit a primary care doctor through GW.
“There are a lot of times, I think, when public health collaborates with medicine either because research questions are clinical or they have clinical implications or they are acts of care issues, they are quality of care,” she said. “There are lots of reasons that collaboration between the two schools is high.”
McCarthy said working with the medical school on research helps advance patient care and health care because what impacts a person’s health isn’t always directly medical. She said areas like education, the environment, nutrition and access to green spaces play a “big role” in someone’s health, and public health research works to address these factors with medical research.
“Collaborating outside of health care on health is very important, especially as we go forward and try to reduce cost,” she said.
McCarthy said funding is already competitive for research projects, and combining different levels of expertise between both schools can make research projects more appealing and more likely to be federally funded. She said the University currently has a cross-disciplinary research funding program – which provides internal funds to at least two different schools to collaborate – but there could be more funding opportunities offered directly from GW.
The fund – which was originally created in 2010 – replaced a fund that promoted work between centers and institute directors in 2016 and now makes any faculty member working on interdisciplinary research eligible for a grant.
Sam Simmens, a research professor of epidemiology and biostatistics, said he currently runs the Milken Institute School of Public Health’s biostatistics consulting service, where “virtually all of the work” is collaborative. He said working with the medical school – in addition to his colleagues within the public health school – can help researchers put together a more complete “picture” of an issue, where more than one approach is considered before starting a project.
“It can result in more creative, innovative results or projects because you are hearing ideas that come from other disciplines that you may not have thought of before,” Simmens said.
Avi Dor, a professor of health policy and management and the director of the health economics program, said one of the most unexpected collaborations between the two schools has been research on health care economics. Dor said the health economics program houses projects that examine the impact of regulatory environments and state policies on both medical practices and public health, which require skill sets from both schools.
Dor said one project currently looks at the impacts of medical malpractice insurance premiums on cardiologists and the type – factoring in the level of risk – of treatments prescribed.
“By joining efforts, together we were able to secure funding from both NIH and foundations to implement this research,” Dor said in an email. “This exemplifies the strong interest in both the biomedical research community and health policy communities nationally in understanding the role financial incentives play in influencing health care.”
Meredith Roaten contributed reporting.